A blood clot in a constricted artery is the primary cause of a heart attack, yet scientists have discovered various other risks that remain unnoticed and believe individuals should be aware of.
Physicians are educated to identify typical arterial obstructions, which are prevalent in elderly individuals with conventional risk factors, yet this emphasis may lead them to overlook less frequent causes since these situations do not align with the anticipated pattern.
The hidden causesfrequently affect young, otherwise healthy people who do not match the typical profile of a heart attack victim.
A 15-year investigation conducted by Mayo Clinic scientists found that over half ofheart attacks among younger individuals, particularly women, result from ‘nontraditional’ factors, meaning numerous root causes remain unidentified and unaddressed.
Dr. Claire Raphael, an interventional cardiologist at the Mayo Clinic and the lead researcher of the study, stated, “This research brings attention to heart attack causes that have traditionally been overlooked, especially in women.”
If the underlying reason for a heart attack is misinterpreted, it may result in therapies that are less effective—or potentially damaging.
Certain elements that scientists identified involved a heart that was excessively strained due to a serious condition such as an infection or internal bleeding, along with an unexpected rupture in the arterial wall.
Scientists also discovered that a heart attack resulting from a serious illness is more than four times deadlier at the five-year point compared to a typical heart attack caused by a blocked artery.

The scientists started by locating all individuals living in Olmsted County, Minnesota, who were 65 years old or younger and experienced a cardiac event between 2003 and 2018, along with increased heart damage indicators; these include chemicals that enter the blood when the heart muscle is injured, such as a protein known as troponin.
Every case was examined separately, with heart attacks, also known as myocardial infarction (MI), classified into one of six distinct causes.
The factors involved were plaque rupture (atherothrombosis), spontaneous coronary artery dissection (SCAD), clot movement (embolism), arterial spasm (vasospasm), non-blocking causes (MINOCA-U), or an imbalance between oxygen supply and demand.
In the long run, cholesterol, fat, and deposits accumulate within the artery walls, a condition that has historically been associated with high blood pressure, elevated cholesterol levels, smoking, diabetes, and a genetic predisposition to heart disease.
If the plaque ruptures abruptly, it leads to the formation of a blood clot that obstructs the artery.
A spontaneous coronary artery dissection (SCAD) refers to an abrupt tear in the arterial wall that does not involve plaque. It commonly occurs in healthy women of young to middle age and is frequently associated with hormonal changes, such as those following childbirth or genetic disorders that affect connective tissues.

An embolism happens when a blood clot develops in another part of the body, commonly as a result of an abnormal heart rhythm such as atrial fibrillation, and then moves to obstruct a coronary artery.
Other factors do not result in any permanent obstruction. A coronary artery vasospasm refers to a brief, intense tightening of the artery that interrupts blood flow, typically caused by smoking, extreme stress, or the use of stimulant drugs.
In conclusion, a supply-demand imbalance (Type 2 MI) arises when the heart is deprived of oxygen because of a significant disproportion under intense physical strain.
A discrepancy may arise during a serious infection, significant blood loss, or an extremely rapid heartbeat, when the heart’s demand for oxygen significantly exceeds what its compromised arteries can provide, even in the absence of a rupture or blockage.
For more than 15 years, Mayo scientists studied 4,116 instances of heart damage in 2,780 individuals aged from their early 40s to mid-60s, with 68 percent attributed to plaque rupture.
The incidence of heart attacks was notably reduced among women, particularly concerning those linked to plaque.
Nevertheless, spontaneous arterial tears occurred 3.5 times more frequently in women and were incorrectly diagnosed at the beginning in 55 percent of cases.
Although women who experienced heart attacks related to plaque were of similar age to men and had comparable levels of arterial disease, they had a higher number of risk factors.
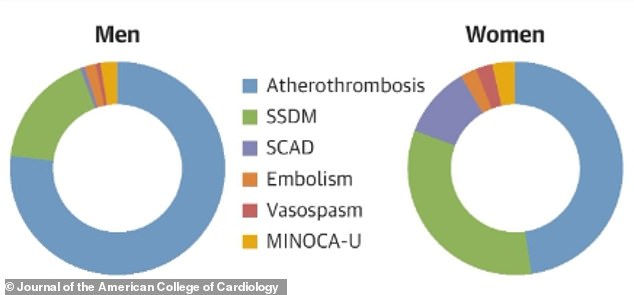
Most heart attacks in women were caused by factors unrelated to plaque, at 53 percent, whereas in men it was 25 percent.
This involved a disparity between supply and demand, impacting 34 percent of women compared to 19 percent of men, and SCAD, which was observed in 11 percent of women versus 0.7 percent of men.
The five-year mortality rate was highest following supply-demand imbalance incidents, with 33 percent passing away by the end of the period, in contrast to eight percent for plaque-related events and zero percent for SCAD.
Mortality related to the cardiovascular system was minimal in all groups.
Dr. Rajiv Gulati, chair of the Division of Interventional Cardiology and Ischemic Heart Disease at Mayo Clinic and the study’s senior author, stated, “Our research underscores the greater importance of reevaluating how we handle heart attacks in this group of patients, especially younger adult women.”
Healthcare professionals need to enhance their understanding of conditions such as SCAD, embolism, and stress-induced factors, while patients should seek clarification when something seems off.
Their results were released in theJournal of the American Heart Association.
Heart attacks were typically associated with older individuals who had a history of risk factors, including obesity and elevated cholesterol levels.
However, currently, one out of five individuals with heart disease is younger than 40. Women often exhibit symptoms that appear unrelated to a heart attack, leading to missed diagnoses.



At just 28 years old, Eve Walker was a vigorous, healthy contemporary dancer with no apparent cause to believe she was vulnerable to a heart attack.
Her overall health seemed very good. She was young, physically active, and had no recognized medical issues.
Nevertheless, she did not realize she had an underlying genetic risk: hypertrophic cardiomyopathy, a disorder that leads to thickening of the heart muscle and may interfere with blood circulation.
Her symptoms were mild and could be confused with other conditions. They started with severe tiredness, like becoming completely out of breath while climbing stairs. A few days later, she experienced a peculiar, moving “pinch” similar to a mosquito bite, which traveled up her leg and side to her face, along with heavy legs and discomfort.
This made her inform a neighbor: “I believe I’m experiencing a heart attack.” The hospital verified this.
The incident resulted in her diagnosis, uncovering a serious inherited heart disorder that had previously led to her sister’s mysterious death years before.
In addition, having a heart attack during one’s 20s or early 30s is increasingly frequent each year. Between 2000 and 2016, the yearly heart attack rate among younger individuals increased by two percent every year.
- What makes heart attacks a sudden danger for young adults, even though their age implies they should be at lower risk?
- Heart attacks during youth: What’s causing this 66% increase among adults in their prime?
- What is causing a growing number of health-aware young adults to suffer sudden, dangerous heart attacks while engaging in everyday tasks?
- Sudden increase in heart attacks among youth: Are teenagers facing a growing danger of these unforeseen incidents?
- Why are heart attacks increasingly prevalent among young, apparently healthy people under the age of 44?




Leave a comment