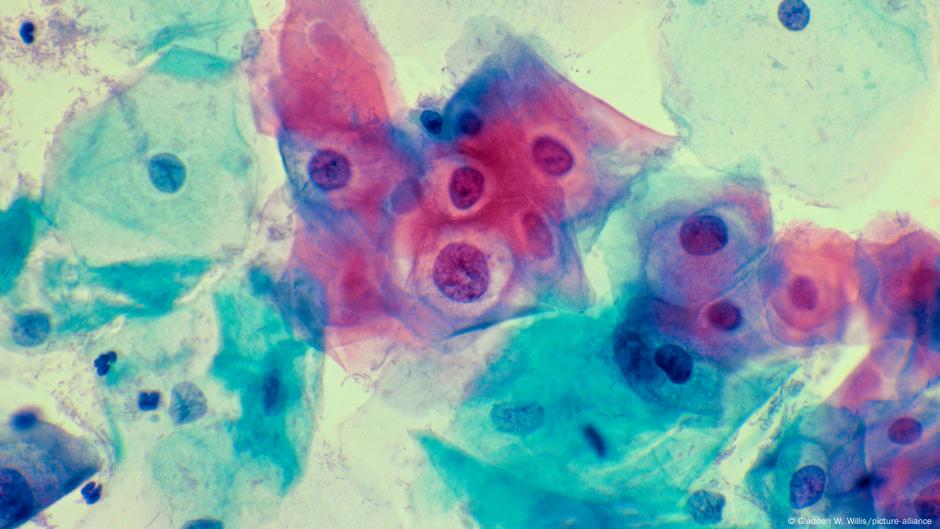
The human papillomavirus (HPV) causes at least 95% of the 660,000 cervical cancer cases reported worldwide. However, studies from the United States highlight the significant effect of continuous vaccination initiatives.
A vaccine given to teenage girls and boys has proven so effective that community protection against a virus responsible for cervical cancer is becoming attainable, particularly in the United States.
Nevertheless, experts state that maintaining community opposition to the human papillomavirus (HPV) will rely on the US’s ability to keep vaccination rates high.
Human papillomavirus (HPV) is the most prevalent sexually transmitted infection globally. Vaccines targeting specific types of HPV, of which there are numerous, have been available for nearly twenty years.
A “nine-valent” vaccine — which offers protection against nine types of HPV responsible for 90% of cervical cancers — is currently approved in the United States. In contrast, other countries utilize vaccines that target two or four specific strains.
Studies released in the magazineJAMA Pediatricshas discovered that the wide-scale HPV vaccination initiative in the United States has led to significant declines in cervical cancer cases, even among women who did not receive the vaccine.
“Our research provides evidence of herd immunity against HPV, which causes cervical cancer, within a specific community, under conditions of high vaccination coverage and a gender-neutral approach to immunization, meaning vaccinating both boys and girls,” said the study’s senior author, pediatrician Jessica Kahn from the Albert Einstein College of Medicine in New York City.
Kahn’s community denotes a particular group of women who are at increased risk for HPV, with nearly 80% having had two or more male sexual partners and over half having received an STI diagnosis.
A review of almost 20 years of data from the group revealed that HPV infections prevented by vaccines dropped significantly. For bivalent vaccines, which cover two strains, there was a 98% reduction in infections.
Since the sexual behaviors of the study group remained largely unchanged, it suggests that HPV vaccines are likely responsible for reducing infection rates, even among women who were not vaccinated. Despite lacking immune protection, this group experienced a 75% decrease in infections caused by the strains targeted by the bivalent vaccine.
This occurrence implies that herd immunity to the illness in the United States may be attainable, although Kahn warned that it would never be possible to confirm with certainty.
There isn’t a particular moment where we can confirm that HPV has been eradicated,” Kahn stated. “Community immunity is constantly changing and may weaken if vaccination rates drop, people become more vulnerable to HPV, or the way it spreads changes.
HPV: Usually harmless, yet possibly life-threatening
Cervical cancer ranks as the fourth prevalent cancer among women, with the majority of fatalities taking place in low and middle-income nations.
The human papillomavirus (HPV) was initially identified as a contributing factor to cervical cancer byGerman scientist Harald zur Hausen in 1983. His findings earned him a shared award of the 2008 Nobel Prize in Medicine.
A significant number of individuals who are sexually active contract HPV at some stage in their lives, yet often do not show any signs. These viruses can lead to the development of skin growths—typically harmless—commonly found on the skin, feet, hands, throat, and genital areas.
In some cases, specific HPV viruses may integrate into healthy cells, interfering with their regular functions. In the cells that cover the cervix, this can result in the formation of cancer.
The incidence of cervical cancer has decreased following the launch of a vaccine known as Gardasil, which was created by scientists in Australia during the 1990s and became available in the 2000s. It marked the beginning of a series of vaccines capable of preventing HPV infections.
Existing HPV vaccines are typically given to girls between the ages of 9 and 14. Boys within this age range can also be vaccinated, as is practiced in the United States, to enhance overall community immunity.
Widespread implementation persists despite obstacles
The World Health Organization (WHO) aims to eradicate cervical cancer as a significant health concern.
The plan aims to ensure that 90% of girls are vaccinated by the age of 15 worldwide, at least 70% of women get cervical cancer screenings by 35 and again at 45, and 90% of women diagnosed with the disease receive treatment.
According to WHO modeling, achieving these goals could avoid 74 million new cervical cancer cases, including 300,000 within this decade.
Extended vaccination initiatives have effectively reduced the incidence of cervical cancer. A study involving over 1.6 million Swedish girls and women revealed almost half the number of cervical cancer cases among vaccinated individuals compared to those who had not received the vaccine.
The principal researcher of that study, Jiayao Lei, an epidemiologist at the Karolinska Institute in Sweden, stated that the results from the US study were not unexpected, based on the findings of her own research.
“It serves as strong evidence since it shows the indirect protection provided by vaccination, especially for those who are not vaccinated [women],” Lei stated.
Lei mentioned that getting vaccinated during teenage years offers enhanced protection from HPV, even if just a single dose is administered.
People who received the vaccine at a younger age will experience stronger protection,” Lei stated. “A similar level of effectiveness is observed in those who were vaccinated earlier [regardless of the dose], whereas for individuals who got vaccinated after the age of 20, it appeared that a higher dose could provide improved protection.
This is especially crucial for nations that are just starting to administer the vaccine to teenagers. Pakistan has recently launched its HPV initiative for girls between the ages of 9 and 14, while Ghana plans to begin providing vaccines to this age group in October.
Still, there are challenges.
Pakistan is facing domestic disinformation efforts, especially in response to false assertions that the vaccine leads to infertility. Nevertheless, nine million girls have already received the vaccine, as reported by Pakistan’s health ministry. The country aims to vaccinate approximately 13 million girls.
The increasing prevalence of vaccine doubt and reduced willingness to get vaccinated worldwide presents a distinct challenge in managing and, ultimately, eliminating diseases such as cervical cancer caused by HPV. Interruptions in vaccination initiatives and health system emergencies, unequal access to vaccines, and reluctance fueled by false information and misleading campaigns create significant obstacles in reducing the incidence of cervical cancer.
“The vaccine works very well, but only when it is administered through injections,” Kahn stated.
Edited by: Rosalie Delaney
Author: Matthew Ward Agius




Leave a comment