By Frank Okello
The World Health Organization (WHO) has warned that antibiotic resistance is spreading quickly, transforming manageable infections into life-threatening conditions and quietly contributing to what specialists now refer to as a “global health emergency.”
Infections that used to be treatable with regular medications are becoming harder to manage. According to WHO data, almost one out of every six bacterial infections is now resistant to typical antibiotics, a concerning situation that puts millions at risk for diseases that were once common.
As per the agency’s most recent monitoring report, resistance to antibiotics increased in over 40% of the bacteria-drug pairs monitored from 2018 to 2023, with average yearly rises varying between five and 15 percent.
The study, drawing on information from more than 100 nations, presents the most detailed view so far of the extent of the issue. It revealed that one out of every three infections in the WHO’s South-East Asia and Eastern Mediterranean regions showed resistance to antibiotics, in contrast to one out of five in Africa.
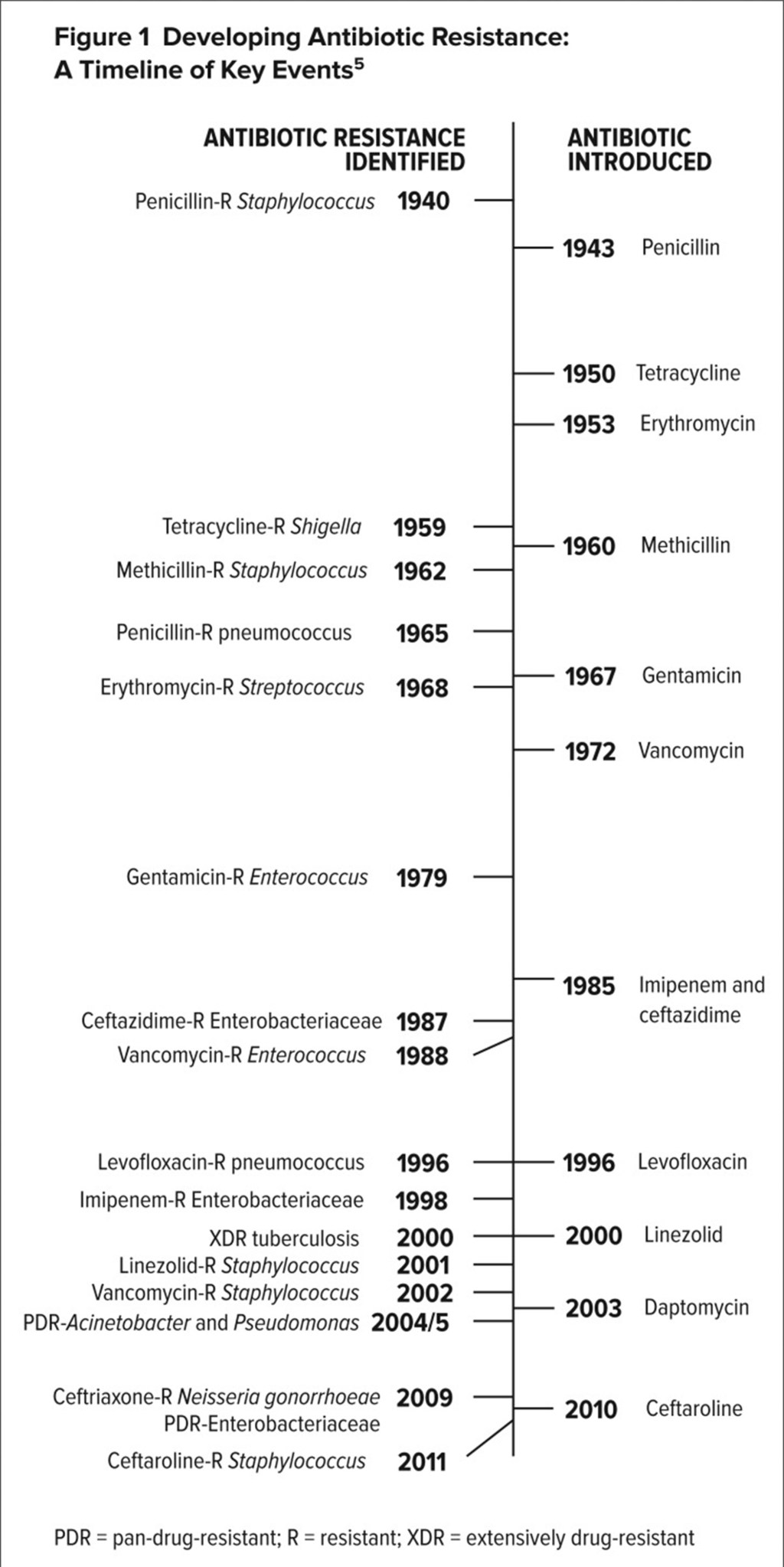
Numerous elements are contributing to this increasing resistance. The excessive and improper use of antibiotics continues to be the primary reason, as numerous individuals consume them without medical prescriptions or for viral conditions where they have no effect.
Limited diagnostic capabilities lead doctors to prescribe broad-spectrum antibiotics “just to be safe.” Inadequate sanitation and poor infection control in overfilled healthcare settings also contribute to the rapid spread of bacteria, while the overuse of antibiotics in animal farming pollutes the food supply.
In the meantime, drug manufacturers, discouraged by minimal financial returns, have mostly stopped working on new antibiotics, resulting in a decreasing number of powerful medications available.
The World Health Organization and international health officials are urging immediate, collaborative efforts. They highlight the “One Health” concept, which acknowledges the link between human, animal, and environmental well-being.
Authorities are being encouraged to enhance control over antibiotics, increase monitoring efforts, and fund studies for innovative medications and other treatments like phages and antimicrobial peptides.
“Since nations are enhancing their Antimicrobial Resistance (AMR) monitoring systems, it is crucial that we use antibiotics wisely and ensure that all individuals have access to the correct medications, reliable diagnostics, and vaccines,” states Tedros Adhanom Ghebreyesus, Director General of the WHO.
Professionals claim that addressing this issue goes beyond policy, requiring public awareness and shifts in behavior. Neighborhoods need to understand that antibiotics are not remedies for all ailments. Appropriate usage, under the direction of medical professionals, can preserve lives over time. Informing agriculturalists and healthcare providers about responsible practices, supporting immunization efforts, and fostering advancements in medical research can together turn the situation around. The World Health Organization cautions that failing to act could lead to disastrous consequences, with millions of deaths each year by 2050 if resistance remains uncontrolled.
Antibiotic resistance goes beyond a health concern; it serves as a challenge for international collaboration and accountability. It poses a risk of reversing years of medical advancements and highlights the vulnerability of contemporary healthcare systems. Each instance of resistant infection is a signal that our collective safety measures are deteriorating.
The crisis might be quiet, but its effects are loud and catastrophic. Only by working together can governments, scientists, industries, and everyday people regain control over this hidden threat before the era of antibiotics becomes a memory.
Provided by SyndiGate Media Inc. (Syndigate.info).




Leave a comment